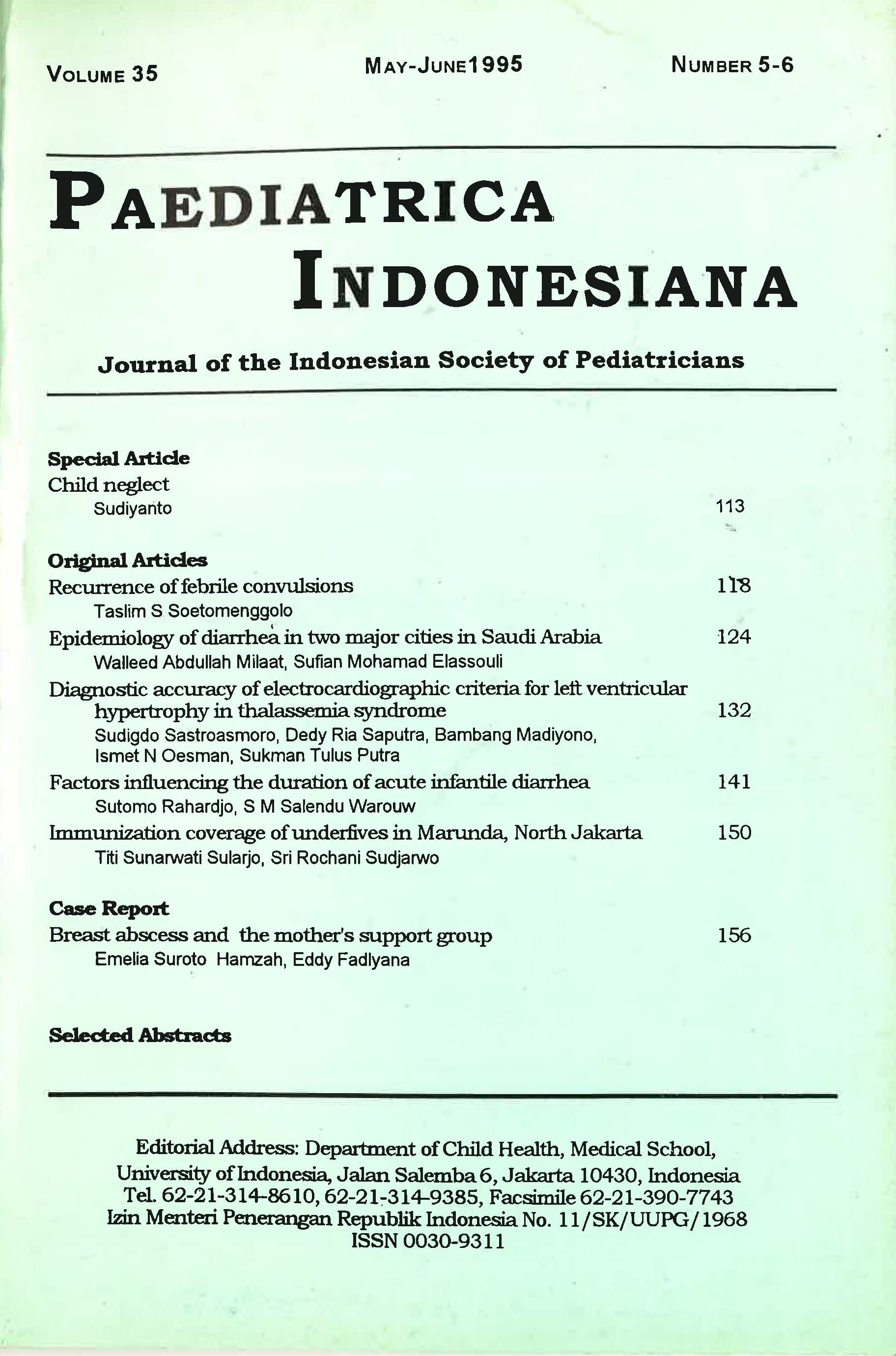
Diagnostic Accuracy of Electrocardiographic Criteria for Left Ventricular Hypertrophy in Thalassemia Syndrome
DOI:
https://doi.org/10.14238/pi35.5-6.1995.132-40Keywords:
electrocardiographic criteria; left ventricular hypertrophy; thalassemia syndrome; echoLVH; BSA indexed; height indexedAbstract
We compared the diagnostic accuracy of electrocardiographic (ECG) criteria for left ventricular hypertrophy (LVH) in 119 randomly selected from 400 patients with thalassemia major treated at the Department of Child Health, Medical School, University of Indonesia, Jakarta. Echocardiographically derived left ventricular hypertrophy (EchoLVH), both for body surface area (BSA)-indexed and height-indexed, served as the gold standard. There were 57 girls and 62 boys available, ranging in age from 5 to 27 years. ECG criteria for LVH was detected in 23 outof119 patients, while echo-LVH was detected in 47 patients if BSA-indexed LVH was used, or 22 patients if height-indexed LVH was used. The sensitivity and specificity of ECG-LVH were 25.5 and 84.7% respectively if BSA indexed LVH was used as gold standard, or 36.4% and 84.5%, respectively, when height indexed echo-LVH was used. It is concluded that ECG criteria for LVH has a low sensitivity and hjgh specificity in detecting increased left ventricular mass in children with thalassemia major.
References
2. Weatherall DJ. The thalassemia, Hematology; 3rd ed. New York: Me Graw-Hill, 1983; 493-517.
3. Keberle H. The biochemistry of desferrioxamine and its relation to iron metabolism. Arm N Y Acad Sci 1964; 119:758- 68.
4. Kaye SB, Owen M. Cardiac arrhythmias in thalassemia major: Evaluation of chelation treatment using ambulatocy monitoring. BrMedJ 1977; 342.
5. Koren A, Garty L. Right ventricular cardiac dysfunction in beta thalassemia major. Am J Dis Child 1976; 141:93-6.
6. Leon MB, Borer JS. Detection of early cardiac dysfunction in patient with thalassemia and chronic iron overload. N Engl J Med 1978; 301:1143-8.
7. Engle MA, Erlandson M, Smith C H. Late cardiac complications of chronic, severe, refractocy anemia with hemochromatosis. Circulation 1964; 30:698-704.
8. Sastroasmoro S, Madiyono B, Oesman IN. Sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy in children with rheumatic heart disease. Paediatr Indones 1991; 31:233-44.
9. Browner WS, Newman TB, Cummings SR. Designing a new study: III. Diagnostic test In: Hulley SB, Cumming SR, eds. Designing clinical research. Baltimore: Wiliiams & Wilkins, 1988; 87-97,
10. Ganong WP. Review of medical physiology; 6th ed. California: Lange Medical Publ., 1973: 200.
H. DevereuxRB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: Comparison of necropsy findings, Am J Cardiel 1986; 57:450-8.
12. Sahn DJ, Demaria A, Kisslo J, Weyman A. The Committee on M-mode Standardization of the American Society of Echocardiography. Recommendations regarding quantitation in M mode echocardiography : result of a survey of echocardiographic measurements. Circulation1978; 58:1072-81.
13. Tarwoljo I, Soekinnan. Status gizi anak. Gizi Indones 1987; 12:6-14.
14. Panitia asuhan nutrisi. Bahan-bahan pelatihan. In: Simposium dan Pelatihan Gizi Klinik. Jakarta 1993.
15. Goldschlager N, Goldman MJ. Principles of clinical electrocardiography; 13th ed. San Francisco: Lange, 1989; 58-72.
16. Silverman NH. Pediatric echocardiography. Baltimore: Wiliiams '& Willcins, 1993; 35-108.
17. Daniels SR, Meyer RA, Liang Y. Echocardiographically determined left ventricular mass index in normal children, adolescents, and young adults. J Am Coll Cardiol1988; 12:703-8.
18. Dawson-Saunders B, Trapp RG. Estimating and comparing proportions. In: Dawson-Saunders B, Trapp RG, ed. Basic and clinical biostatistics. East Norwalk: Appleton & Lange, 1990; 142-60.
19. Morris JA, Gardner MJ. Calculating confidence inteiVals for relative risks, odds ratios, and standardized ratios and rates. In: Gardner MJ, Altman, ed. Statistics with confidence. London: Br Med J,
1989; 50-2.
20. Heruy WL, Nienhuis AW, Wiener M, Miller DR, Canale VC, Piomelli S. Echocardiographic abnormalities in patients with transfusion dependent anemia and secondary myocardial iron deposition.
Am J Med 1978; 64:54 7-55.
21. Dewi LP. Profil pertumbuhan jasmani pada pasien talasemia mayor. Tesis. Jakarta: Bagian Ilmu Kesebatan Anak FKUI, 1992.
22. Sinulingga S, Loebis IF, Sutjipto A. The pattern of thalassemia in children at the Department of Child Health, School of Medicine Universizy of North Sumatera/Dr Pirngadi Hospital, Medan. Paediatr Indones 1991; 31:261-7.
23. Devereux RB. Is the electrocardiogram still useful for detection of left ventricular hypertrophy? Circulation 1990; 81: 1144-6.
24. Levy D, Labib SB, Anderson KM, Christiansen JC, Kannel WB, Castelli WP. Determinants of sensitivizy and specifily of electrocardiographic ctiteria for left ventricular hypertrophy. Circulation 1990; 81:815-20.
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following terms:
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.